American Society of Clinical Oncology ASCO 2019
ASCO 2019 : Metaplastic Breast Cancer Global Alliance
Chicago, IL : May 31st– June 4th 2019Meeting for American Society of Clinical Oncology
Chicago, IL : May 31st– June 4 2019
The Metaplastic Breast Cancer Global Alliance was excited to qualify for an ASCO-Sponsored Patient Advocacy Booth this past May 31st through June 4th, 2019. This annual meeting of the American Society of Clinical Oncology provides nonprofit patient organizations the opportunity to meet, interact and exchange information with approximately 40,000 meeting attendees from all over the globe.
Florida -- 22
here
South Carolina -- 4
here
Georgia -- 8
here
Alabama -- 2
here
North Carolina -- 4
here
Tennessee -- 3
here
Mexico --
here
Texas--25
here
New Mexico -- 4
here
Arizona -- 3
here
Utah -- 1
here
California -- 23
here
Oregon -- 4
here
Montana -- 2
here
South Dakota -- 1
here
Minnesota -- 4
here
Iowa -- 5
here
Illinois -- 14
here
Wisconsin -- 5
here
Michigan - 11
here
New York -- 10
here
New Jersey -- 8
here
Pennsylvania -- 10
here
Maryland -- 5
here
Washington State -- 3
here
Virginia -- 8
here
South Africa -- 1
here
Costa Rica --
here
Romania -- 1
here
Germany -- 3
here
Netherlands -- 1
here
New Hampshire -- 1
here
Kentucky -- 4
here
Indiana -- 8
here
Greece - 2
here
Poland - 1
here
Ohio-- 5
here
Missouri--3
here
Colorado--7
here
Nebraska--3
here
Curacao--1
here
Louisiana--3
here
Spain--1
Connecticut -- 1
Hawaii-- 1
West Virginia-- 1
Maine-- 2
Massachusetts--1
Puerto Rico--1
Mississippi--1
Kansas--1
Philippines--1
Ontario Canada-- 6
Manitoba Canada-- 2
Alberta Canada-- 2
Toronto Canada-- 2
Newfoundland Canada-- 1
Quebec Canada -- 0
British Columbia Canada-- 0
Saskatchewan Canada-- 0
New Brunswick Canada-- 0
Nova Scotia Canada-- 0
Prince Edward Island, Canada-- 0
Nunavut, Canada--0
Northwest Territories Canada--0
Yukon Canada --0
British Columbia Canada--0
Western Australia--4
Northern Territory Australia--0
South Australia--0
Queensland Australia--8
New South Wales Australia--2
Victoria Australia--2
Tasmania Australia--0
New Zealand--2
Malta--1
India-- 1
Scotland, United Kingdom --
Northern Ireland, United Kingdom
Wales, United Kingdom -- 1
England, United Kingdom -- 17
Republic of Ireland -- 1
Alaska -- 1
India -- 1
Singapore -- 1
Turkey -- 1
We were able to share our Diagnosed Member Map at our Booth from a LapTop.

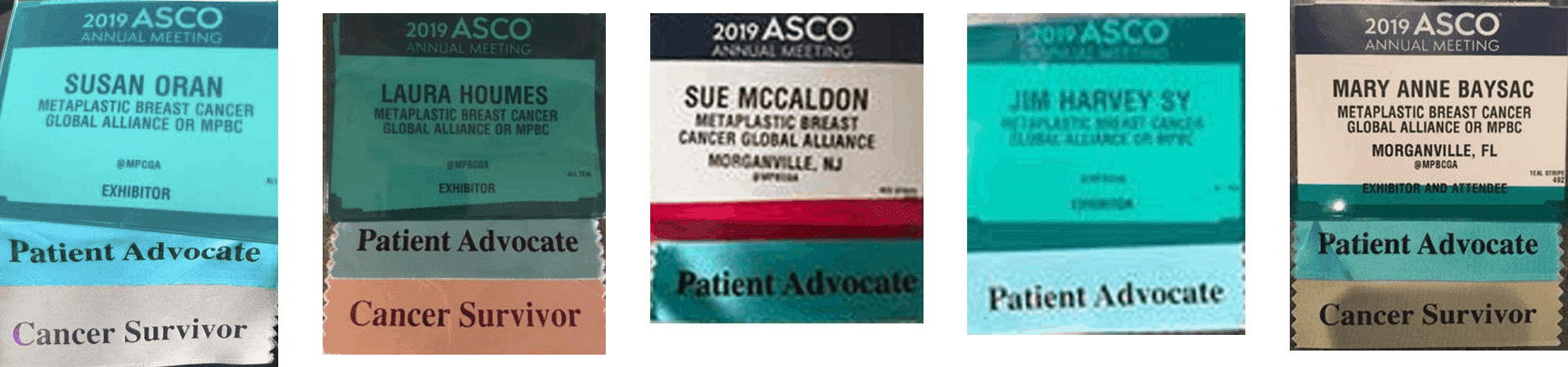
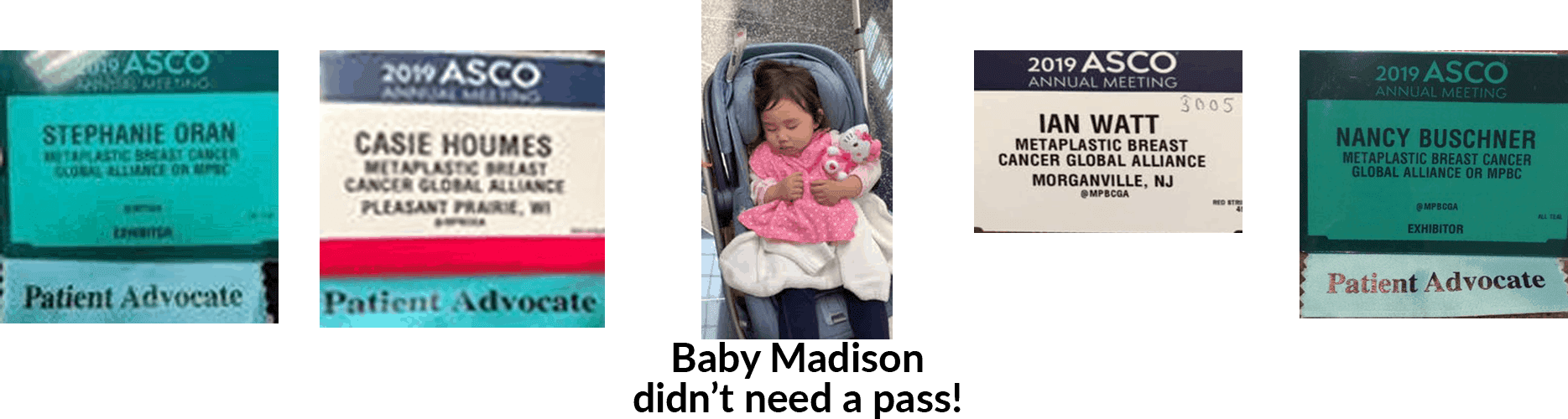
Members, Family and Friends
We were very fortunate to have ten diagnosed members, family and friends attend this valuable conference and assist our busy booth. We were thrilled with the welcome we received from doctors all over the world who were surprised to see a patient advocacy group representing MpBC! We shared information with many doctors and even made a short video with a doctor from Brazil so that she could provide better support to her patients!

“Raising Global Awareness and Supporting Research for Metaplastic Breast Cancer”

Our handouts:


Continued Need for Research
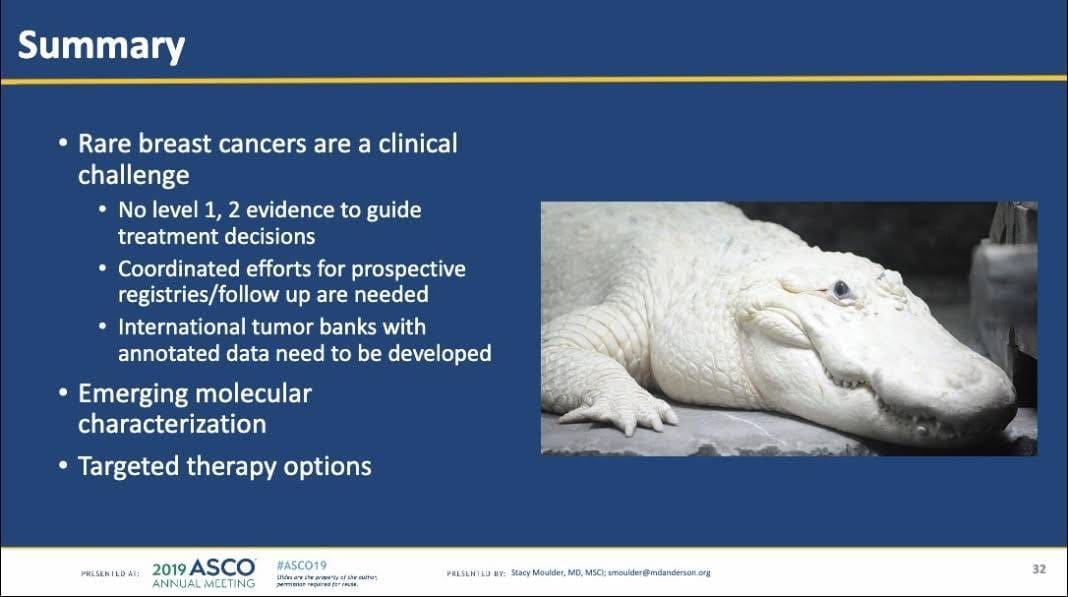
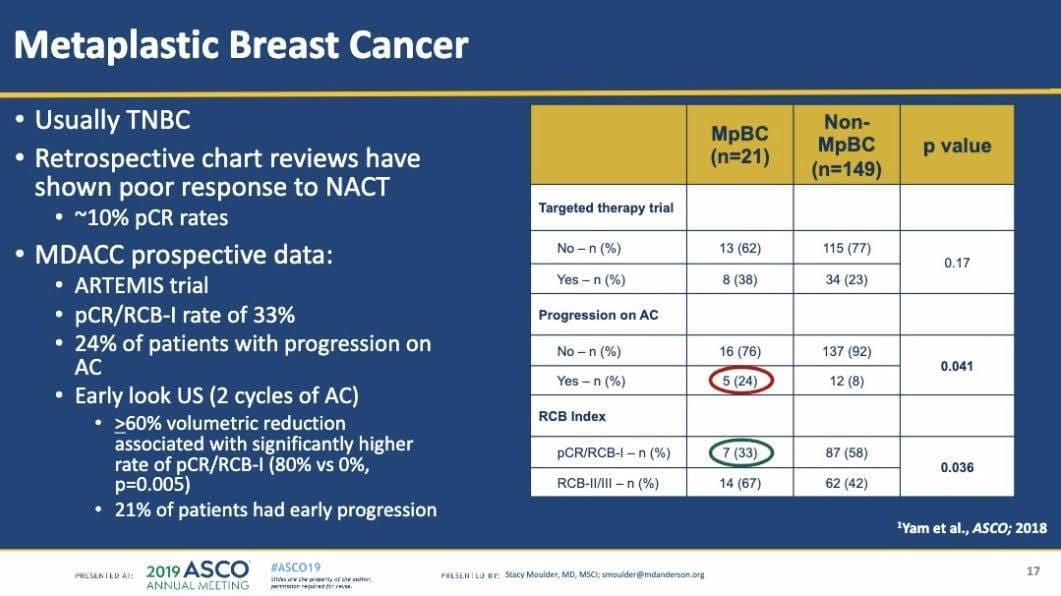
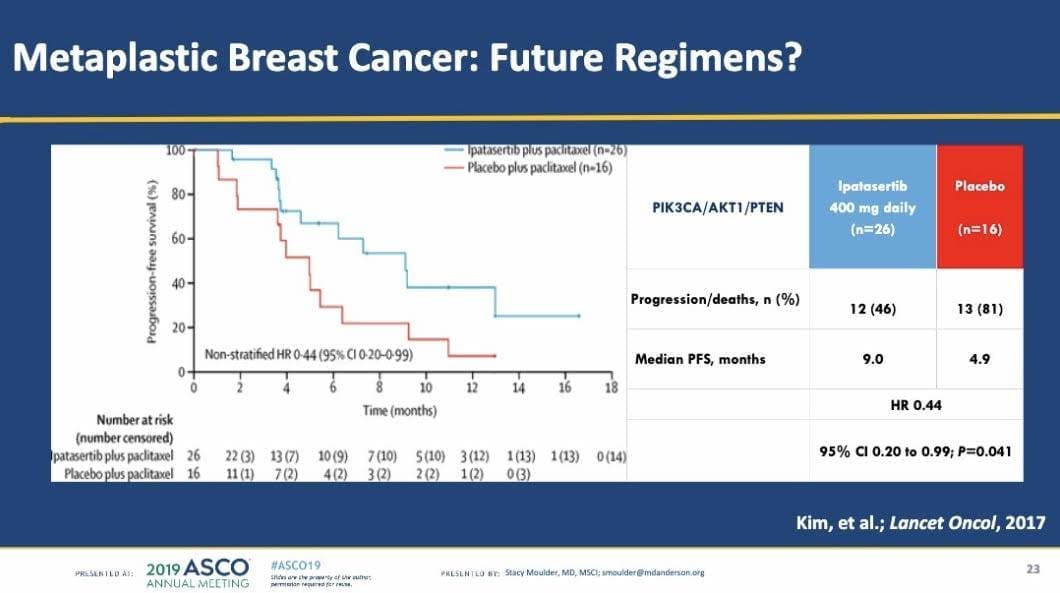
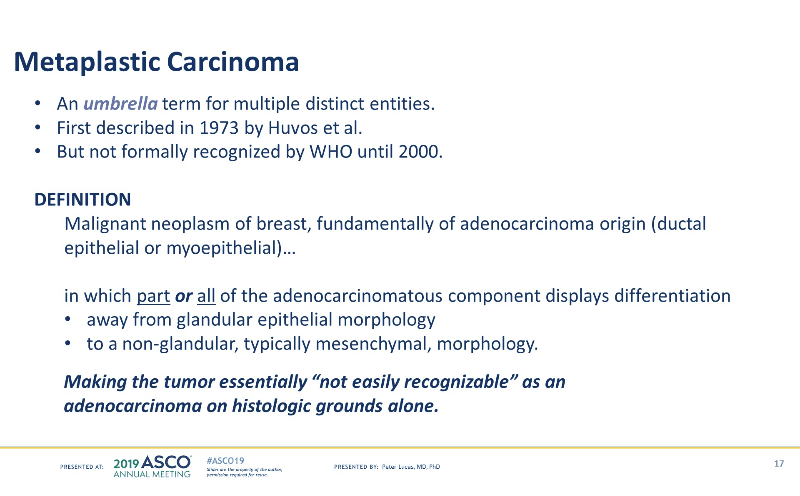
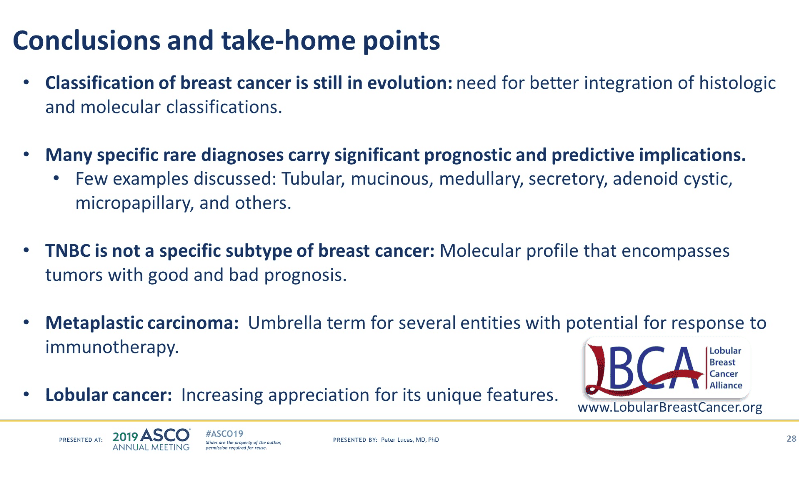
The week was capped off by an early-morning session on Monday the last day of the conference, delivered by Dr. Stacey Moulder, that highlighted Metaplastic Breast Cancer and the need for research.
ASCO is the largest venue for sharing cutting edge scientific and educational developments in oncology and we were very proud of all our efforts and how we represented our rare community.


Meeting with Dr. Moulder at our Booth

Other Patient Advocates We Met

Ian Still Sporting Our Shirt!
Best Memories and Takeaways from ASCO 2019!

Susan D. Oran– “For me, the highlight was hearing Metaplastic Breast Cancer discussed in a session attended by hundreds of doctors at 8am and meeting with Dr. Moulder again. Eating dip-n-dots with my oncologist Dr. Michael Nissenblatt and meeting all of you wonderful people and seeing how we were able to ban together towards our common goals so easily!”

Nancy McCormack Buschener– “Meeting all of you and your amazing doctors. I learned so much! Oh and the cake building!”

Sue McCaldon– “For me it was meeting you all and having the opportunity to go into sessions to learn so much. Also, seeing my doctor and finding my drug trial poster and talking to the research people in the drug company.”

Dr. Janku stopped by to say Hi!
Jim Harvey Sy– “Best part was meeting you guys and learning that there is so much out there focused on finding a cure for cancer”

Casie Friedrich- “For me it was seeing oncologists and other oncology professionals from all around the world looking to us for information to better help their patients! And the Lattes with your face on them!”

Stephanie Oran– “Hearing Dr. Moulder say that social media has provided a way for doctors to meet patient advocacy groups (like us!) Oh and all the free snacks!”
Laura Houmes– “My first takeaway is WOW! I am completely exhausted but was worth all our combined efforts. I can’t say there was any “best” part of our ASCO gathering. The whole event was a blessing to me and more than I could have imagined. Metaplastic breast cancer brought us all together and we all are trying to make a difference. I believe we made all who have donated to our nonprofit proud!”
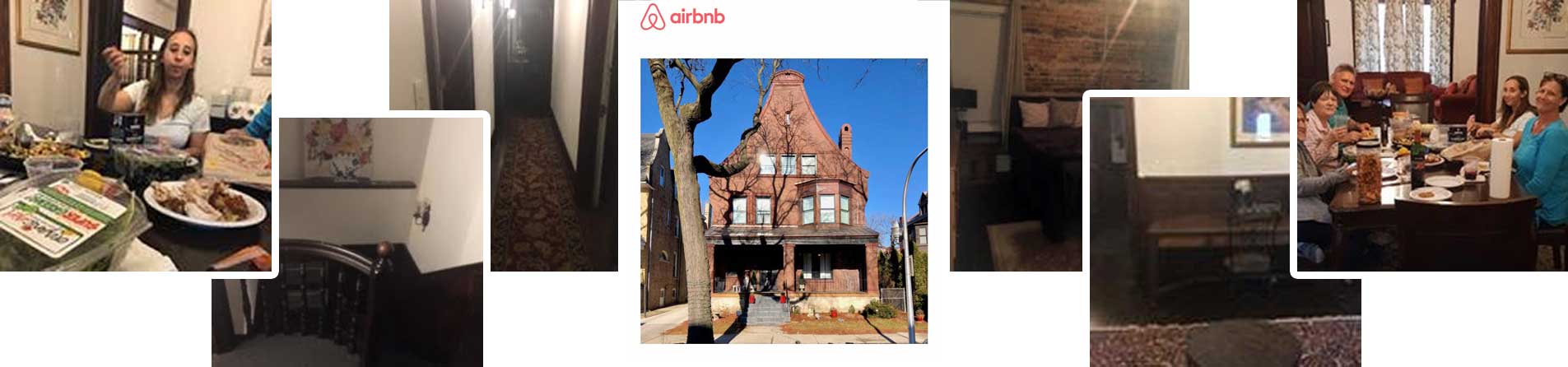
Finally, just some images from our time at a local historical, 1800s haunted AirBnB!